Are you prone to experiencing migraine, and have you ever wondered if low blood sugar might be to blame?
You're not alone; many people experience headaches or migraines triggered by drops in blood glucose levels. The important role of energy metabolism and hypoglycemia in migraine is getting more and more attention recently.
Understanding this connection is crucial for managing your health and finding effective support.

Low blood sugar, or hypoglycemia, can trigger a cascade of reactions in the body, including hormonal changes, increases of oxidative stress (free radicals) and energy deficiency in the brain, all of which may lead to headaches and migraine.
Recognizing the symptoms of low blood sugar and understanding how they relate to migraine attacks can empower you to take control of your well-being.
In this article, we will explore the mechanisms that link low blood sugar to migraine, discuss how to identify potential triggers, and provide practical strategies to prevent blood sugar dips.
With this knowledge, you can make informed decisions about your diet and lifestyle to reduce the frequency of migraine and enhance your overall quality of life.
Keep reading to uncover vital information that can help you manage migraine caused by low blood sugar effectively!
Blood Sugar Crashes as Migraine Triggers
You're likely aware that low blood sugar can trigger migraine by initiating specific physiological mechanisms:
Brain's Dependence on Glucose:The brain relies on glucose as a vital source of energy. When blood sugar levels drop too low, the brain is deprived of fuel, leading to neurological and physiological changes that may trigger migraines.
Activation of Stress Responses:Low blood sugar activates the sympathetic nervous system (the "fight or flight" response). This leads to the release of stress hormones like adrenaline and cortisol, which can contribute to migraine onset by:
Increasing blood pressure.
Constricting or dilating blood vessels, which affects blood flow in the brain.
Increasing oxidative stress
Release of Excitatory Neurotransmitters:Hypoglycemia stimulates the release of glutamate, an excitatory neurotransmitter. Excessive glutamate activity can cause overexcitation of neurons, a potential factor in the initiation of migraines.
Impact on Serotonin Levels:Fluctuations in blood sugar can affect serotonin levels. Serotonin plays a role in regulating blood vessel tone, and imbalances can lead to vasodilation or vasoconstriction, both of which are associated with migraine.
Triggering Cortical Spreading Depression (CSD): The energy deficit caused by low blood sugar may increase susceptibility to cortical spreading depression (CSD), a wave of neural hyperactivity followed by inhibition that is thought to underlie migraine aura and headaches.
Increased Sensitivity to Other Triggers: Hypoglycemia can lower the body's threshold for other migraine triggers, such as stress, dehydration, or hormonal fluctuations.
Symptoms of Hypoglycemia and Migraines Overlap
Both hypoglycemia and migraines can cause symptoms like:
Fatigue.
Irritability.
Difficulty concentrating.
Nausea. This overlap may make it difficult to differentiate between the two conditions initially.
Recognizing common signs, such as mood changes or sweet cravings, can help you manage these episodes effectively and prevent migraine onset.
How Low Blood Sugar Activates Migraine Mechanisms
When blood sugar levels drop, you experience a blood sugar imbalance, prompting the brain to signal for more glucose.

This demand often results in the release of stress hormones, which can lead to migraine headaches.
The physiological mechanisms behind this involve the dilation and constriction of blood vessels, a reaction that commonly occurs during migraine episodes.
Symptoms of hypoglycemia, such as fatigue, confusion, and mood changes, often precede these headaches.
Your brain requires a constant energy supply, and when deprived, it can't function optimally, leading to these debilitating symptoms, which can be seen as a warning signal that there is an energy shortage and a means to force us to rest until energy reserves are restored.
Addressing this requires careful dietary management to maintain stable blood sugar levels.
Incorporating regular, balanced meals with low glycemic index foods into your diet can help prevent the rapid blood sugar fluctuations that trigger migraine.
Common Signs of Blood Sugar Related Migraines
Early indicators of an impending migraine due to low blood sugar, or hypoglycemic episodes, often include yawning, sweet cravings, sweating, and mood changes.
You might also notice a dull, throbbing sensation in your temples, blurred vision, or an elevated heart rate.
It's crucial to address these signs as soon as they appear to prevent a full-blown migraine.
Low blood sugar in migraine can be a result of reactive hypoglycemia.
Reactive hypoglycemia is a condition where blood sugar levels drop too low within 2–4 hours after eating, typically due to an excessive release of insulin in response to a meal.
This often happens after consuming foods high in refined carbohydrates, which cause a rapid spike and subsequent sharp decline in blood sugar.
Symptoms may include shakiness, fatigue, hunger, sweating, irritability, anxiety, and difficulty concentrating.
Managing reactive hypoglycemia involves eating smaller, balanced meals throughout the day that include protein, healthy fats, and complex carbohydrates to stabilize blood sugar levels and avoid rapid spikes and drops.
Consuming a balanced snack with protein, fat and carbohydrates can stabilize your blood sugar levels quickly.
Regular monitoring of your glucose levels can help you recognize patterns and avoid triggers.
Prevention strategies like maintaining a consistent meal schedule and selecting low glycemic index foods or even low carb foods or ketogenic diets can significantly reduce migraine occurrences.
Additionally, ensuring adequate sleep and managing stress are essential components of any comprehensive migraine treatment plan.
By staying vigilant and prepared, you can reduce the frequency and severity of migraine caused by low blood sugar, improving your overall quality of life.
The Science Behind Sugar-Induced Head Pain
When your blood sugar dips, the physiological mechanisms kick in, causing your brain to struggle without adequate glucose.
Such episodes are closely tied to migraine and glucose-related traits, as your body's response includes releasing stress hormones and altering blood flow.
These changes can constrict blood vessels, a hallmark of migraine auras.
Insulin resistance can exacerbate these issues, as it affects how your body manages glucose.
When your insulin isn't functioning efficiently, maintaining stable blood sugar becomes challenging.
This instability plays a significant role in triggering migraine.
Research shows that specific glycemic traits, like fasting insulin levels, are linked to migraine, suggesting a genetic component.
Smart Eating to Prevent Sugar Drop Migraines
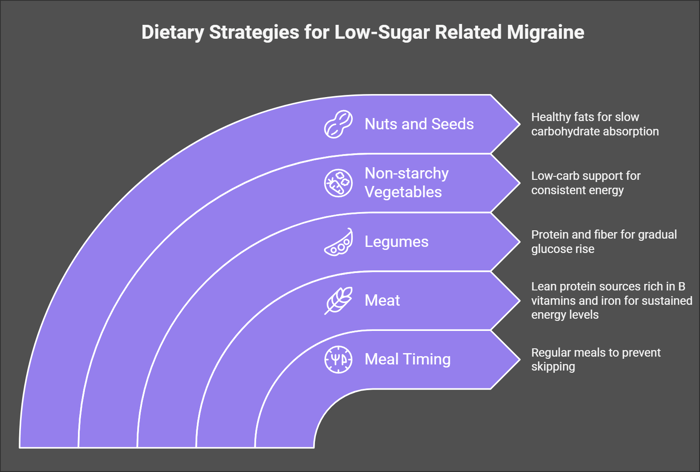
To effectively prevent migraine triggered by low blood sugar, it's essential to focus on meal timing and food choices.
Eating regular, balanced meals with real foods and at least low glycemic index foods like protein, meat, vegetables and lower carb fruits and nuts helps maintain stable blood sugar levels, minimizing the risk of migraine attacks.
Some patients benefit further from reducing carbohydrates drastically and going into ketosis.
Ketosis is a metabolic state where the body primarily burns fat for energy instead of carbohydrates.
This occurs when carbohydrate intake is very low, causing the liver to produce ketone bodies from fat to supply energy, especially for the brain, as an efficient and alternative energy source.
This can be achieved via a ketogenic diet, a high-fat, very low-carbohydrate diet designed to induce ketosis: in this fasting mimicking state the liver will produce this alternative energy source in the absence or scarcity of glucose.
Typically, a ketogenic diet includes about 70-80% of calories from fat, 10-20% from protein, and 5-10% from carbohydrates. It requires careful planning to maintain nutritional balance.
More recently, an alternative means of getting into ketosis is via supplementation. Ketone bodies being produced in the lab to be added on a (hopefully healthy) diet, without a super strict ketogenic diet.
The main options are between ketone body esters (ketone bodies bound to an alcohol) and ketone body salts (ketone bodies bound to a mineral).
As alcohol is not great for liver function and migraine, we strongly recommend ketone body salts, as can be found in MigraKet.
Timing Your Meals for Migraine Prevention
Avoid meal skipping, as it can lead to fasting-related migraine, a common issue for many sufferers.
By eating at regular intervals, you can maintain stable blood sugar levels, reducing the likelihood of an attack.
Dietary management plays a critical role in this strategy. Aim to consume meals every three to four hours to keep energy levels steady.
Breakfast is particularly important; don't skip it. A balanced morning meal can set the tone for your blood sugar stability throughout the day.
Consider having a small, healthy snack before bed if morning headaches are frequent, as this can help maintain glucose levels overnight.
Best Foods That Keep Blood Sugar Stable
Meal timing plays a vital role in stabilizing blood sugar levels to effectively manage migraine.
Incorporating the right foods into your diet is essential for maintaining blood sugar within a healthy range and preventing migraine triggered by low blood sugar.
Focus on dietary management with foods that promote blood sugar regulation and include protein, fats and other foods with with a low glycemic index (GI).
Here are some foods to consider:
Meat, eggs and other protein: Meat protein sources include lean options like chicken, turkey, and fish, as well as red meats like beef, pork, and lamb, all of which provide high-quality, complete proteins rich in essential amino acids and basically zero carbohydrates. If tolerated eggs can also be a great option.
Legumes: Beans, lentils, and chickpeas are rich in both protein and fiber, promoting a gradual rise in blood sugar. Their low GI makes them ideal for preventing sugar drops.
Non-starchy Vegetables: Vegetables such as broccoli, spinach, and bell peppers are low in carbohydrates and have a minimal impact on blood sugar levels, supporting consistent energy supply.
Nuts and Seeds: Almonds, walnuts, and chia seeds provide healthy fats and protein, which slow down carbohydrate absorption and further aid in blood sugar regulation.
Incorporating these foods into your meals can aid in managing migraine linked to low blood sugar.
Dangerous Foods That Spike and Crash
Simple carbohydrates can be particularly problematic, as they often lead to rapid spikes and subsequent crashes in blood sugar levels.
Foods high in these carbohydrates, like white bread, sugary snacks, and sodas, can increase your risk of migraine by causing significant fluctuations in glucose levels.
Understanding the glycemic traits of these foods is crucial for effective dietary management.
When you consume simple carbohydrates, your body quickly converts them into glucose, leading to a temporary surge in energy.
However, this is often followed by a sudden drop, which can trigger blood sugar headaches and increase the risk of migraine.
To manage your dietary intake and maintain stable glucose levels, focus on complex carbohydrates and low glycemic index foods, such as whole grains and legumes.
Migraine Support When Sugar Drops Strike
When a sudden drop in blood sugar triggers a migraine, quick action with emergency food solutions such as a 15g sugary snack can help stabilize blood sugar levels.
Following the initial response, a post-attack recovery strategy should include rest, hydration, and a balanced meal to restore energy.
If symptoms persist or become severe, seeking medical support is crucial to prevent further complications.
Emergency Food Solutions for Quick Help
Emergency management is crucial in these situations to stabilize your condition and avert migraine attacks.
Begin by consuming a 15g sugary snack to quickly elevate your blood sugar.
This could be a small glass of fruit juice, a spoonful of honey, or a few pieces of candy.
Such simple carbohydrates are absorbed rapidly, providing an immediate energy boost to your brain.
Following the sugary snack, it's important to consume a protein, fat and carbohydrate-rich snack to maintain and stabilize blood sugar levels.
Combining protein and carbohydrates helps sustain energy release, preventing another drop.
Consider these quick solutions:
Peanut Butter and Fruit: Offers a balanced mix of proteins and carbs.
Cheese and Whole-Grain Bread: Provides lasting energy with a healthy combination of nutrients.
Yogurt with Fruit: Delivers immediate sugars with sustaining proteins.
Trail Mix with Nuts and Dried Fruit: Combines fast-acting sugars with longer-lasting energy sources.
These strategies ensure you're prepared to tackle low blood sugar episodes effectively, minimizing the risk of triggering a migraine.
Post-Attack Recovery Strategy
After a migraine attack triggered by low blood sugar, it's crucial to focus on recovery and restoring your body's equilibrium.
Understanding the role of postprandial hypoglycemia in migraine occurrences can guide your strategy.
Begin by rehydrating with mineralized water, as your body loses minerals when you lose glucose (=glycogen) stores and consuming a balanced meal that includes complex carbohydrates, fat and proteins to stabilize glucose levels.
Recognize that glucose-related traits can influence your response to dietary interventions, so tailor your approach accordingly.
Incorporate treatment strategies that emphasize dietary management.
Opt for meals that sustain blood sugar without causing sharp spikes or drops.
Proteins, and healthy fats, vegetables and if tolerated complex carbohydrate sources can provide steady energy release, reducing the likelihood of another migraine.
Pay attention to portion sizes and meal timing to mitigate postprandial hypoglycemia effects.
Additionally, recovery isn't just about what you eat—it's about how you rest and rejuvenate.
Adequate sleep and stress reduction techniques like mindfulness or gentle yoga can aid in restoring balance.
When to Seek Medical Support
If you're insulin resistant or experiencing frequent migraine linked to low blood sugar, it's crucial to consult a healthcare provider.
They can offer insights into prophylactic treatments and preventive measures tailored to your needs.
Consider seeking medical support if:
Migraine Frequency Increases: If you're experiencing migraine more than a few times a month, it might indicate an underlying issue that requires medical attention.
Severe Symptoms: When migraine are accompanied by severe symptoms like confusion, loss of consciousness, or persistent vomiting, it's essential to seek immediate help.
Ineffective Management: If your current strategies aren't working and low blood sugar continues to trigger migraine, a healthcare professional can help adjust your treatment plan.
Concerns About Insulin Resistance: If you suspect insulin resistance is affecting your blood sugar levels, professional evaluation can guide you to appropriate interventions.
Proactively addressing these issues with your healthcare provider ensures you're on the right path to effectively manage migraine and maintain stable blood sugar levels.
Building Your Anti-Migraine Lifestyle
To build an anti-migraine lifestyle, focus on daily habits that stabilize blood sugar, such as consuming balanced meals with low glycemic index foods or even trying a ketogenic or low carbohydrate diet.
Daily Habits That Stabilize Blood Sugar
By focusing on dietary management, you can effectively implement prevention strategies to minimize migraine occurrences.
Consistent habits ensure that your lifestyle considerations align with maintaining stable blood sugar levels. Here's how you can make a difference:
Regular Meals: Eating balanced meals at consistent times helps regulate blood sugar. Incorporate proteins and healthy fats to avoid spikes and crashes.
Low Glycemic Index Foods: Choose foods that release glucose slowly, like vegetables and legumes or protein sources and fat sources that do not contain much glucose at all. These options support steady energy levels and decrease migraine risk.
Mindful Snacking if needed: Prevent blood sugar dips by consuming small, nutritious snacks between meals. Opt for combinations like nuts and fruit to sustain energy and avoid hunger-induced migraine.
Whole foods and nutrients: Opt for whole foods full of nutrients and add nutrients supplementary if needed.
Adequate Sleep: Prioritize quality sleep to bolster blood sugar regulation. Sleep deprivation can disrupt glucose metabolism, increasing migraine susceptibility.
Watch out for Allergens: Eating foods that you are not tolerating will increase blood sugar via a stress response. Test whether you might be intolerant to gluten, dairy or other food items, which could also set you up for failure.
Ketogenic diet: If all of this is not enough, a whole foods ketogenic diet, which is high in fat and very low in carbohydrates, may further help stabilizing blood sugar levels and reducing brain inflammation. This diet also promotes the production of ketone bodies, which provide an alternative energy source for the brain and may help with migraine triggers related to glucose metabolism.
Medical Food Support for Enhanced Migraine Support
Beyond basic dietary management, specialized medical foods like MigraKet can provide additional support for blood sugar stability and provide an alternative energy source in the form of ketone bodies..
This Swiss-developed all-in-one migraine support works through multiple mechanisms:
MigraKet offers a multifaceted approach to migraine management through four essential pillars that address potential root causes of blood sugar or energy deficiency-related migraine:
Pillar | Function | Benefits | Implementation |
Blood Sugar Stabilization | • Supports glucose metabolism • Enhances insulin sensitivity • Maintains steady energy levels | • Reduces frequency of blood sugar crashes • Helps prevent hypoglycemia-triggered energy deficit • Supports consistent brain energy supply | • Take as directed with or after meals • Monitor blood sugar patterns • Combine with balanced meals |
Antioxidant Protection | • Combats oxidative stress • Protects mitochondrial function • Supports cellular health | • Potentially reduces inflammation • May protect brain cells from damage • Enhances energy production efficiency | • Regular daily intake • Consistent long-term use • Combine with antioxidant-rich foods |
Micronutrient Support | • Provides essential vitamins • Delivers key minerals • Supports enzymatic functions | • Optimizes metabolic processes • Enhances nutrient absorption • Supports overall brain health | • Follow recommended dosage • Take with food for better absorption • Monitor nutrient levels with healthcare provider |
Alternative Energy Sources | • Provides ketone bodies • Give the brain an alternative energy source to glucose • Enhances metabolic flexibility | • Offers backup energy source when glucose is low • Improves brain energy efficiency • Reduces dependence on glucose alone | • Consistent daily intake • Take during key metabolic windows • Use as part of regular routine |
This comprehensive approach addresses long-term support by:
Supporting optimal brain metabolism
Maintaining stable energy levels
Minimizing oxidative stress
Providing essential nutrients for cellular function
For best results, integrate this medical food support with:
Regular meal timing
Proper hydration
Stress management
Adequate sleep
Regular exercise
Exercise Without Triggering Crashes
Physical activity can induce hypoglycemia and thereby trigger migraine, so it's crucial to approach exercise without triggering hypoglycemic crashes.
To prevent these crashes, you'll want to balance exercise and activity with proper dietary management and hydration.
Start by ensuring you're well-fed before engaging in exercise. Incorporate a snack rich in complex carbohydrates, fats and protein about 30 minutes before activity to maintain blood sugar levels.
Stay hydrated, too, as dehydration can exacerbate both blood sugar imbalances and migraine symptoms.
Aim to drink water regularly and consider electrolyte supplements (or MigraKet) if needed.
Time | Action | Purpose |
Pre-exercise | Snack (fats+ carbs + protein) | Stable blood sugar and enough energy |
During | Hydration (water/electrolytes) | Prevent dehydration |
Post-exercise | Balanced meal (proteins/carbs) | Replenish energy stores |
After exercise, a balanced meal helps replenish energy and stabilize blood sugar.
Prevention strategies include monitoring how different exercises affect your blood sugar.
Low to moderate-intensity workouts are less likely to cause significant drops.
Adjust your exercise routine based on your experiences and consider consulting a healthcare professional to optimize your activity plan.
Sleep and Stress Management Tools
Balancing exercise with proper dietary management sets the stage for an effective anti-migraine lifestyle, but equally important are sleep and stress management tools.
These tools are crucial in stabilizing blood sugar levels and reducing migraine frequency.
Ensuring consistent sleep patterns helps regulate your body's glucose metabolism, reducing the risk of hypoglycemia-induced migraine.
Stress can trigger fluctuations in blood sugar, so managing stress effectively is essential. Here are some practical strategies:
Prioritize Sleep Hygiene: Establish a regular sleep schedule by going to bed and waking up at the same time daily. This consistency supports your body's natural circadian rhythms and helps maintain stable blood sugar levels.
Incorporate Relaxation Techniques: Practices like deep breathing, meditation, or yoga can significantly reduce stress, thereby minimizing its impact on blood sugar and potential migraine triggers.
Monitor Your Stress Levels: Use tools like journals or apps to track stress triggers and responses. Understanding these patterns can guide you in developing personalized stress management strategies.
Seek Professional Support: A therapist or counselor specializing in stress management can provide valuable guidance and techniques tailored to your needs, helping you maintain an anti-migraine lifestyle.
Implementing these tools can enhance your overall well-being and significantly lower migraine occurrences.
Frequently Asked Questions
After exploring the topic of migraine caused by low blood sugar, you may still have some questions.
We’ve compiled a list of frequently asked questions to provide clarity on this subject.
What's the genetic link between insulin resistance and migraine?
Research has identified several genetic factors, including variations in the insulin receptor gene, that can affect both insulin production and migraine susceptibility.
These genetic links help explain why some families have a higher prevalence of both conditions.
Studies show that mutations affecting endothelial cells and insulin signaling pathways can influence both glucose metabolism and cerebral blood flow, potentially increasing migraine risk.
How does the menstrual cycle affect the relationship between blood sugar and migraine?
Hormonal fluctuations during the menstrual cycle can affect both insulin sensitivity and migraine susceptibility.
Changes in estrogen levels can influence glucose metabolism and impact how adipose tissue responds to insulin, potentially leading to temporary peripheral insulin resistance.
This combination of hormonal and metabolic changes can increase the likelihood of blood sugar-related migraine during certain phases of the menstrual cycle.
Can people with diabetes distinguish between low blood sugar headaches and true migraine?
While both conditions can cause head pain, there are distinct differences.
Low blood sugar headaches in people with diabetes typically resolve quickly with the administration of insulin or glucose correction, while true migraine persist even after blood sugar returns to the normal range.
Additionally, migraine often come with specific neurological symptoms that aren't typically present in simple low blood sugar headaches.
How do proinsulin levels and glycemic traits influence migraine frequency?
Elevated proinsulin levels can indicate insulin resistance and metabolic dysfunction, which may increase susceptibility to both episodic migraine and chronic migraine.
Specific glycemic traits, such as fasting glucose variability and post-meal glucose responses, can affect the inflammatory response in the body and influence migraine frequency.
What role does cognitive impairment play in the relationship between blood sugar fluctuations and migraine?
During episodes of low blood sugar, temporary cognitive impairment can occur, which may serve as both a warning sign and a compounding factor in migraine development.
The brain's reduced ability to process information and maintain normal function during these episodes can trigger a cascade of events leading to active migraine.
This connection is particularly important for understanding how secondary headaches develop in relation to blood sugar fluctuations.
How does excessive sugar intake affect the history of migraine in susceptible individuals?
Regular high sugar intake can lead to increased inflammation, oxidative stress and changes in cerebral blood flow, potentially worsening the history of migraine in susceptible individuals.
This pattern can create a cycle where metabolic disruptions and the action of insulin become increasingly dysregulated, leading to more frequent and severe migraine episodes. Understanding this relationship is crucial for long-term migraine management.
Conclusion
Managing blood sugar-related migraine comes down to smart dietary choices and lifestyle habits.
By maintaining regular meal times, choosing the right whole foods, and staying prepared with emergency snacks, you can significantly reduce migraine frequency.
Remember that proper sleep, stress management, and professional medical support when needed are also key components of an effective migraine prevention strategy.
With these tools in hand, you can take control of your migraine and improve your daily life.





