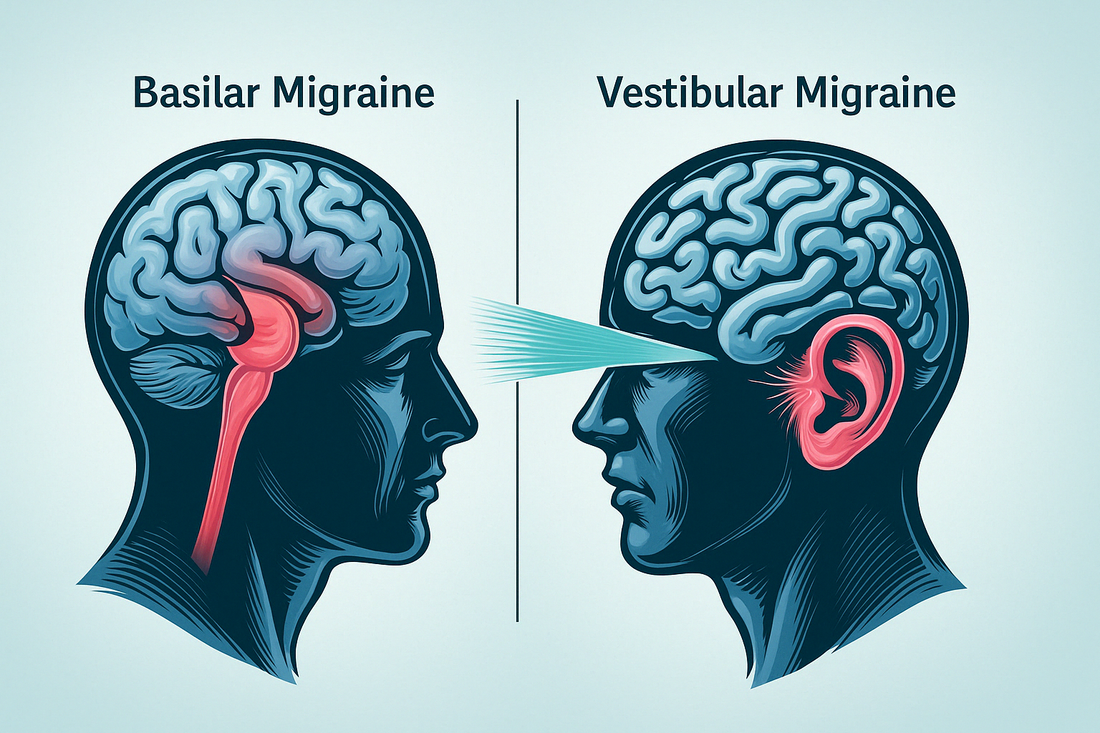
Basilar Migraine vs Vestibular Migraine: Key Differences Explained
Are you experiencing dizziness, vertigo, or balance problems with your migraine?
You might be dealing with either basilar or vestibular migraine—two conditions that often get confused but require different approaches.
The truth is, these specific migraine types can dramatically affect your daily life, sometimes even without severe headache pain.
Basilar migraine (now officially called migraine with brainstem aura, or MBA) involves your brainstem and can cause frightening symptoms like slurred speech, double vision, and severe vertigo.
Vestibular migraine, on the other hand, primarily targets your inner ear's balance system, leading to dizziness and spatial disorientation that can last for days.
Why does knowing the difference matter? Because it’s the first step towards getting the right help.

If you've been struggling with these symptoms without clear answers, this article will help you understand exactly what sets these conditions apart, what to discuss with your doctor, and which protocols are most likely to bring help for your specific situation.
Brainstem Aura vs Inner Ear migraine
When comparing brainstem aura (basilar) and inner ear (vestibular) migraine, you'll find that the origins of neurological symptoms differ significantly, impacting diagnostic criteria and protocol strategies.
Origins of Neurological Symptoms
Although both migraine with brainstem aura (MBA) and vestibular migraine manifest as debilitating neurological conditions, their origins distinctly differ in terms of anatomical pathways and mechanisms.
In MBA, neurological symptoms arise from electrical dysfunction within the brainstem, characterized by neuronal depolarization leading to dysarthria, vertigo, and other brainstem-specific symptoms.
MBA typically involves alterations in brainstem activity during an acute attack, causing widespread neuronal disturbances.
Conversely, vestibular migraine originates from the inner ear's vestibular system, leading to vestibular attacks marked by vertigo, dizziness, and balance disruption.
These symptoms occur as the vestibular system processes and integrates sensory inputs, modulating pain and spatial orientation.
Understanding these distinct origins is essential for accurate diagnosis and tailored migraine management strategies.
Aura Characteristics and Requirements
Given their distinct origins, the aura characteristics and requirements for brainstem versus inner ear migraine differ significantly, necessitating precise diagnostic criteria.
Migraine with brainstem aura (MBA) mandates at least two brainstem aura symptoms like dysarthria or vertigo during migraine episodes.
In contrast, vestibular migraine primarily involves vestibular symptoms such as vertigo or balance issues, which might not involve classic aura.
Diagnosing vestibular migraine requires association with migraine features in at least 50% of vestibular episodes.
Severity and Neurological Involvement
Understanding the severity and neurological involvement of brainstem versus inner ear migraine is crucial for accurate diagnosis and management.
Migraine with brainstem aura (MBA) exhibits more pronounced neurological symptoms such as dysarthria and diplopia, reflecting significant brainstem dysfunction.
These symptoms often signal a severe migraine phase, complicating diagnosis and protocol.
In contrast, vestibular migraine primarily affects the inner ear, manifesting as vertigo without the extensive neurological involvement seen in MBA.
Although both conditions share common migraine features, MBA's neurological symptoms necessitate careful evaluation to differentiate it from other disorders.
Diagnosis and aid strategies hinge on recognizing these differences, as MBA requires targeted interventions to address brainstem dysfunction, whereas vestibular migraine protocol focuses on managing vestibular symptoms and associated migraine features.
Vertigo Variations in Migraine Types
When comparing basilar migraine and vestibular migraine, you'll find distinct vertigo characteristics within each type.

Basilar Migraine Vertigo Features
Basilar migraine, or migraine with brainstem aura (MBA), exhibits distinct vertigo features that differentiate it from other migraine types.
It involves recurrent vertigo episodes linked to brainstem-originating issues.
These vertigo episodes are often accompanied by visual disturbances, such as diplopia and bilateral visual symptoms.
Unlike vestibular migraine, where vestibular symptoms dominate the clinical picture, MBA vertigo is part of a broader spectrum of migraine symptoms, including ataxia and decreased consciousness.
The recurrent vertigo in MBA is typically more severe and associated with additional neurological manifestations.
Vestibular Migraine Vertigo Features
In contrast to basilar migraine's neurological complexity, vestibular migraine focuses on a distinct array of dizziness patterns that impact the vestibular system.
You're dealing with episodes characterized by vertigo and dizziness, often triggered by head movements, visual stimuli, or certain beverages—with alcohol and migraine having a particularly strong connection in many patients.
These symptoms can be spontaneous or positional, lasting anywhere from minutes to days.
Unlike migraine with aura, vestibular migraine doesn't necessarily involve visual disturbances before the onset of dizziness.
Understanding these symptoms is crucial for accurate diagnosis and protocol options.
Protocol typically involves migraine-specific medications, vestibular sedatives, and antiemetics to alleviate vertigo and nausea.
Protective strategies include lifestyle modifications and standard migraine aid such as amitriptyline or propranolol.
Such targeted approaches help manage symptoms and improve quality of life.
Duration and Frequency Differences
Although both migraine with brainstem aura (MBA) and vestibular migraine involve vertigo, they differ significantly in the duration and frequency of these episodes.
In MBA, vertigo episodes typically coincide with the aura phase, lasting around 60 minutes (typically lasts between 5 to 60 minutes) before transitioning to the headache phase.
The frequency of episodes varies, often presenting multiple times a year, but not as frequently as vestibular migraine.
Conversely, vestibular migraine features episodes lasting from 5 minutes to 72 hours (vestibular migraine episodes are indeed highly variable), often occurring more frequently.
Common symptoms like dizziness and nausea can disrupt daily life, yet their episode duration and frequency of episodes differ markedly between the two conditions.
Understanding these differences aids in accurate diagnosis and tailored management, ensuring better outcomes for those affected by these distinct migraine types.
Diagnostic Challenges and Distinctions
When distinguishing between basilar migraine and vestibular migraine, you'll encounter several diagnostic challenges due to overlapping symptoms.
Basilar Migraine Criteria
Understanding the diagnostic criteria for migraine with brainstem aura (MBA) presents a unique set of challenges due to its nuanced symptomatology and overlap with other neurological conditions.
You'll need to distinguish basilar-type migraine by identifying brainstem aura symptoms, such as dysarthria, episodic vertigo, and diplopia.

These symptoms must occur in at least two episodes without motor weakness.
The International Classification of Headache Disorders (ICHD-3) provides a framework, yet the episodic nature complicates diagnosis.
Exclusion of other disorders is vital. When dealing with MBA, it's crucial to carefully select migraine medications, avoiding triptans and ergotamines due to potential risks.
Vestibular Migraine Identification
Identifying vestibular migraine presents unique challenges distinct from migraine with brainstem aura.
You must rely on specific diagnostic criteria focused on vestibular symptoms rather than aura.
As partially mentioned above, these criteria include at least five episodes of moderate or severe vertigo, dizziness, or balance issues lasting 5 minutes to 72 hours.
Acute management necessitates using migraine-specific medications or vestibular sedatives to address symptoms like vertigo and nausea.

Unlike migraine with brainstem aura, vestibular migraine doesn't require aura symptoms.
Excluding other vestibular disorders becomes critical, given its prevalence and symptom overlap.
Accurate identification ensures good acute management and long-term protective strategies, enhancing patient outcomes.
Differential Diagnosis Considerations
Despite the overlapping symptoms between migraine with brainstem aura (MBA) and vestibular migraine, distinguishing between these conditions requires careful consideration of their unique diagnostic criteria and symptomatology.
To accurately establish a differential diagnosis, consider these factors:
-
Symptoms and Episodes: MBA often involves visual symptoms and brainstem aura preceding migraine attacks, while vestibular migraine is primarily characterized by vestibular disorders and positional vertigo without auras.
-
Frequency and Onset: MBA typically presents with less frequent but more severe episodes, while vestibular migraine exhibits recurrent episodes of vertigo, often triggered by head movement.
-
Associated Conditions: Vestibular migraine is strongly linked with other vestibular disorders like benign paroxysmal positional vertigo, whereas MBA is more isolated in terms of associated conditions.
Accurate differentiation guides appropriate management strategies.
Tailored Management Approaches
When managing migraine with brainstem aura (MBA) and vestibular migraine, a tailored approach is crucial due to the distinct pathophysiological mechanisms and symptom profiles of each condition.
Pharmacological Management
The pharmacological strategies for these conditions share some similarities but require important distinctions.
Calcium channel blockers like verapamil and flunarizine can be valid for MBA minimization, specifically addressing the neuronal hyperactivity linked with this migraine disorder.
These medications help stabilize the brainstem neurons that become hyperexcitable during attacks.
For vestibular migraine, first-line medications often include beta-blockers such as propranolol and metoprolol, which have shown efficacy in reducing both the frequency and severity of attacks.
Anticonvulsants like topiramate may benefit both conditions, though dosing might differ based on the predominant symptoms.
In acute protocol, traditional migraine medications such as NSAIDs and acetaminophen can help both conditions, but caution is warranted with vasoconstrictive medications like triptans and ergotamines in MBA due to theoretical concerns about basilar artery effects.
These same medications may be safer options for vestibular migraine when appropriate.
Non-Pharmacological Interventions
Beyond medications, both conditions benefit from comprehensive lifestyle modifications.
For MBA, consistent sleep patterns and stress management techniques are particularly important in reducing brainstem sensitivity.
Cognitive behavioral therapy has shown promise in helping patients manage the anxiety that often accompanies the fear of severe neurological symptoms.
Vestibular migraine patients often benefit from vestibular rehabilitation therapy, which can significantly improve their ability to compensate for vestibular symptoms.
These specialized exercises help retrain the brain to process balanced information more efficiently.
Meanwhile, vestibular migraine might require strategies targeting vestibular neuritis-like symptoms, ensuring that protocol approaches don't disrupt daily activities.
Dietary Considerations
Dietary triggers can play a significant role in both conditions but may manifest differently.
For MBA patients, tyramine-containing foods and alcohol can provoke more severe brainstem symptoms.
A detailed elimination diet followed by careful reintroduction can help identify specific triggers.
Vestibular migraine patients commonly report sensitivity to dietary sodium, with fluctuations potentially exacerbating inner ear fluid dynamics and vestibular symptoms.
Maintaining consistent hydration and moderate sodium intake may help stabilize these symptoms.
Multidisciplinary Approach
It's vital to differentiate between these conditions to apply specific interventions that mitigate symptoms and minimize recurrences.
Evidence-based guidelines stress individualized care plans, integrating pharmacological options with lifestyle modifications.
A multidisciplinary approach involving neurologists, otolaryngologists, and vestibular therapists often provides the most comprehensive care for these complex conditions.
Regular follow-up and protocol adjustments are essential, as both conditions may evolve over time and respond differently to interventions.
Patient Education and Self-Management
Empowering patients with knowledge about their specific migraine subtype is crucial for solid management.
MBA patients should be educated about recognizing brainstem aura symptoms that might precede severe attacks, allowing for earlier intervention.
For vestibular migraine sufferers, understanding how to modify activities during prodromal symptoms can prevent falls and injuries related to sudden vertigo.
Maintaining a detailed symptom diary can help both patients and clinicians identify patterns and triggers specific to their migraine subtype.
Here is a comparative table showcasing MBA vs. vestibular migraine:
|
Protocol Aspect |
Migraine with Brainstem Aura (MBA) |
Vestibular Migraine |
|
First-line |
Calcium channel blockers (verapamil, flunarizine) |
Beta-blockers (propranolol, metoprolol) |
|
Second-line |
Anticonvulsants (topiramate, valproate), tricyclic antidepressants |
Anticonvulsants, tricyclic antidepressants (amitriptyline) |
|
Acute Protocols |
NSAIDs, acetaminophen; caution with triptans/ergotamines |
NSAIDs, triptans, antiemetics, vestibular suppressants |
|
Non-pharmacological Approaches |
Sleep hygiene, stress management, consistent meal timing |
Vestibular rehabilitation therapy, balance training |
|
Dietary Management |
Avoid tyramine, MSG, alcohol, aged cheeses |
Moderate sodium intake, consistent hydration |
|
Physical Activity |
Moderate aerobic exercise with caution during prodrome |
Graduated vestibular adaptation exercises |
|
Specialist Involvement |
Neurologist, headache specialist |
Neurologist, otolaryngologist, vestibular therapist |
|
Monitoring Parameters |
Frequency of brainstem aura symptoms, headache intensity |
Vertigo episodes, dizziness severity, functional impact |
|
Contraindicated Protocols |
Vasoconstrictive agents, certain hormonal therapies |
Medications that exacerbate vestibular symptoms |
|
Prognosis Factors |
Frequency of brainstem symptoms |
Degree of vestibular compensation, chronicity |
Recognizing the unique characteristics of each migraine type enables precision in management, enhancing quality of life and minimizing the functional impact on patients.
The goal of protocols in both conditions extends beyond symptom reduction to include functional improvement and minimization of disability.
With appropriate differentiation and targeted therapy, most patients can achieve significant improvement in their condition and maintain their quality of life despite these challenging neurological disorders.
Frequently Asked Questions
You might still have some lingering questions about the differences between basilar and vestibular migraine.
In this section, we address some common and complex questions to help clear up any confusion.
Can physical activity trigger both basilar and vestibular migraine?
While both conditions can be triggered by physical activity, they respond differently.
Basilar migraine sufferers often report that intense exercise or sudden movements can precipitate an attack with brainstem symptoms.
For vestibular migraine patients, even moderate physical activity that changes head position can trigger vertigo episodes.
Exercise modification strategies differ between the conditions, with vestibular migraine patients typically benefiting from gradual vestibular rehabilitation exercises, while those with basilar migraine may need to avoid certain high-intensity activities altogether.
How does sensitivity to light differ between basilar and vestibular migraine?
Photophobia occurs in both basilar and vestibular migraine but manifests differently.
In basilar migraine, it can be accompanied by temporary bilateral vision loss or visual field defects due to occipital cortex involvement during aura.
In vestibular migraine, bright lights and visual stimuli, such as moving patterns, can trigger or worsen vertigo and dizziness, likely due to altered integration of visual and vestibular inputs.
While visual disturbances in basilar migraine are often aura-related and more cortical, vestibular migraine is characterized by heightened sensitivity to environmental visual triggers. These differences reflect varying neurological pathways but overlap significantly depending on the individual.
Are there differences in how monosodium glutamate affects basilar vs vestibular migraine?
There is no strong scientific evidence to suggest that monosodium glutamate (MSG) affects basilar and vestibular migraines through distinctly different mechanisms.
While MSG is reported as a trigger for some migraines due to its interaction with glutamate receptors and potential overstimulation of neural pathways, its effects are not subtype-specific.
Both basilar and vestibular migraines involve overlapping neurological mechanisms, including brainstem and central nervous system dysfunction, and MSG’s role is likely part of a broader sensitivity rather than a targeted effect.
Claims that MSG selectively impacts brainstem nuclei in basilar migraines or vestibular pathways in vestibular migraines remain speculative and are not supported by current research.
How can you distinguish between paroxysmal vertigo episodes and these migraine types?
Benign paroxysmal vertigo episodes can be confused with both migraine types but have distinctive characteristics.
These episodes typically last seconds to minutes, unlike the longer duration of vestibular migraine attacks (hours to days) or basilar migraine aura (typically under an hour).
Additionally, paroxysmal vertigo is often triggered by specific head position changes and resolves quickly, unlike migraine-related vertigo which is usually more persistent.
Diagnosis requires careful attention to accompanying symptoms—basilar migraine includes multiple brainstem symptoms, vestibular migraine may have migraine features without aura, while paroxysmal vertigo typically occurs in isolation without headache or other neurological symptoms.
Is there a different risk of stroke associated with basilar vs vestibular migraine?
Yes, there may be a slight difference in stroke risk between basilar migraine and vestibular migraine, but the distinction is not as significant as it might seem.
Basilar migraine, classified as a type of migraine with aura, carries a slightly elevated stroke risk due to general vascular factors like endothelial dysfunction and hypercoagulability, especially in the posterior circulation. This risk is further increased by smoking and the use of estrogen-containing contraceptives.
Vestibular migraine, on the other hand, has minimal direct evidence linking it to an increased stroke risk, as it is less commonly associated with aura and vascular involvement.
However, stroke risk in both conditions ultimately depends more on the presence of aura, individual risk factors, and vascular health, rather than the specific migraine subtype.
How do barometric pressure changes affect these different forms of migraine?
Barometric pressure changes are a well-known migraine trigger, but the specific mechanisms remain unclear and are not definitively linked to differences between basilar migraine and vestibular migraine.
Both types of migraine may react to pressure fluctuations due to heightened sensitivity in the central nervous system.
Vestibular and non-headache symptoms, such as dizziness or vertigo, may occur in vestibular migraine patients, but this is likely due to central processing dysfunction rather than barometric sensing mechanisms in the vestibular system.
What role does the menstrual cycle play in basilar vs vestibular migraine?
Hormonal fluctuations during the menstrual cycle, particularly estrogen withdrawal before menstruation, play a role in both basilar migraine and vestibular migraine.
There is no strong evidence that these subtypes are affected differently by the menstrual cycle.
Basilar migraines, like other migraines with aura, may cluster premenstrually, but broader relationships to the menstrual cycle are variable.
Similarly, vestibular migraine patients may experience vertigo at different points in the cycle, including ovulation, though this is not unique to this subtype.
Hormonal strategies, such as continuous birth control, can stabilize estrogen levels and may be helpful for patients with hormone-sensitive migraines regardless of subtype. Treatment must be tailored to the individual rather than based on migraine subtype.
How do these migraine types compare to classic migraine and cluster headaches?
Unlike classic migraine (migraine with typical aura), which primarily features visual aura symptoms followed by head pain, basilar migraine involves multiple brainstem symptoms and bilateral visual disturbances.
Vestibular migraine often occurs without any aura but with prominent vestibular symptoms.
Cluster headaches, in contrast, involve severe, unilateral orbital pain with autonomic features like tearing and nasal congestion, typically without the vertigo central to both basilar and vestibular migraine.
Protocol approaches differ significantly, with oxygen therapy being good for cluster headaches but not for either migraine type discussed here.
Conclusion
Understanding the distinct characteristics of migraine with brainstem aura and vestibular migraine is essential for accurate diagnosis and help.
While both fall under the migraine spectrum, their fundamental differences in neurological origin, symptom presentation, and protocol responses significantly impact patient care.
Basilar migraine involves the brainstem, producing severe neurological symptoms like dysarthria, diplopia, and vertigo, often with bilateral manifestations.
In contrast, vestibular migraine primarily affects the inner ear's vestibular system, causing pronounced dizziness and balance disruptions without necessarily involving classic aura.
These distinctions matter not just for diagnosis but for protocol approaches as well.
From medication selection to lifestyle modifications, differentiating between these conditions ensures patients receive targeted interventions that address their specific neurological pathways involved.
With proper identification and management, patients with either condition can experience improved quality of life and reduced symptom burden.
